Overview:
pelvic floor muscles :The term (pelvis) literally means a basin. It is made up of four bones: two hip (innominate) bones, sacrum, and coccyx, bound to each other by the ligaments.
The pelvic floor muscles refer to a group of muscles that support important organs in pelvis like bladder, bowel, and internal reproductive organs. Its allow body to absorb outside pressure (from lifting, coughing, etc.) in a way that protects spine and organs. This is composed of the pelvic diaphragm, which extends from the symphysis pubis anteriorly to the coccyx posteriorly, forming a hammock-like structure which supports pelvic organs. In addition, its help control bowel and bladder function (continence function).
pelvic floor muscles form the base of a core muscles group, which include pelvic floor muscles, abdominal muscles, back muscles, and diaphragm. These muscles attach to pelvis and spine, creating stability throughout body’s center.
pelvic floor muscles stretch from pubic bone in the front of body to coccyx in the back. The muscles extend outward on both sitting bones (ischial tuberosity) on the right and left sides of pelvis. Several pelvic floor muscles intertwine to form a single sheet of layered muscle with openings (anus, urethra, vagina).
The feeling of pelvic floor muscles can be When squeeze these three openings: vaginal opening, Urethra, Anus.
The deep pelvic floor muscles include:
- levator ani muscles.
- coccygeus muscles (Ischiococcygeus)
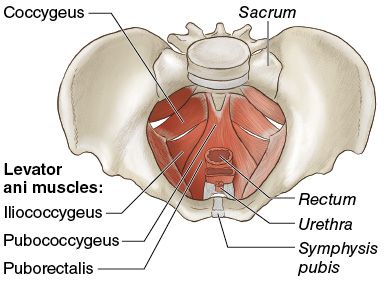
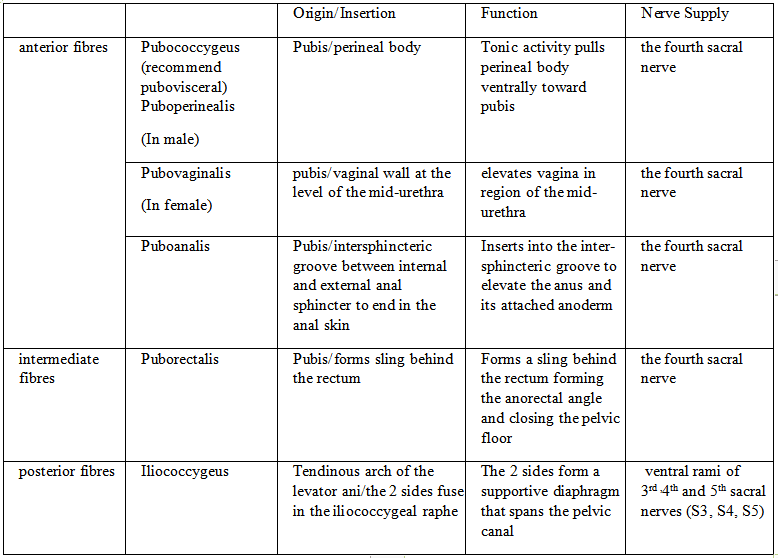
levator ani muscles:
Largest and most important muscle of the pelvic floor and play an essential role in support of the pelvic organs, The two levator ani muscles are the wide curved, thin sheets of muscles. They slope from the side wall of the pelvis toward the median plane where they fuse with each other to form the gutter-like floor of the true pelvis, and separates it from the ischiorectal fossae. it consists of:
coccygeus muscles (Ischiococcygeus):
The coccygeus is a small triangular muscle situated behind the levator ani muscle.
Origin:
It arises by its apex from the pelvic surface of ischial spine and sacrospinous ligament.
Insertion:
From its base into the sides of upper two pieces of coccyx and the last piece of sacrum.
Nerve Supply:
It is by the ventral rami of 4th and 5th sacral nerves (S4, S5).
Actions:
1. The coccygeus muscles assist the levator ani muscles to support the pelvic viscera.
2. They can also produce minor movements of the coccyx.
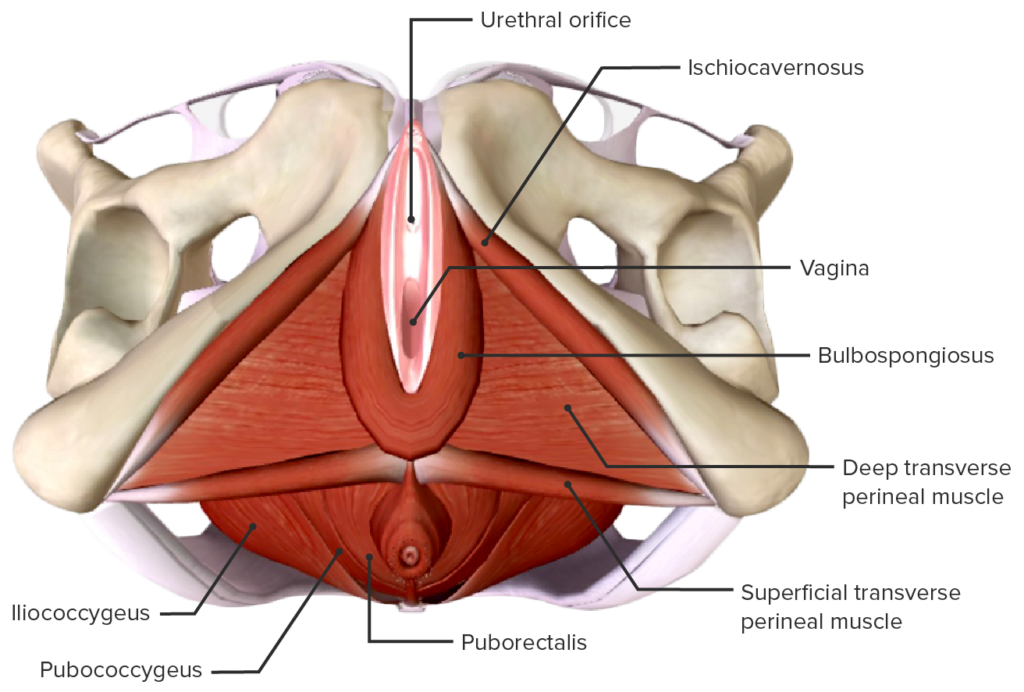
The superficial pelvic floor muscles (known as the urogenital diaphragm), include:
- the bulbospongiosus
- ischiocavernosus
- superficial and deep transverse perineal muscles
- fascial layers, and urethral and anal sphincters.
- The perineal body or central perineal tendon is the convergence of the superficial pelvic muscles and sphincters and provides support to the pelvic floor.
- The obturator internus and piriformis muscles are muscles of the pelvic side walls and externally rotate the femur.
Evaluation of pelvic floor muscles:
In general physiotherapy practice, it is necessary to evaluate the state of the muscle at rest and during a maximum voluntary contraction, this involves inspection, palpation and testing the muscle, and some methods to standardized recording to allow comparison of clinical data before and after treatment. This methodology also applied to the pelvic floor muscles.
1.Inspection:
the pelvic floor muscles are responsible for maintaining both fecal and urinary continence, and the genitoanal area should be inspected to evaluate the skin condition, muscle tone and presence of prolapse.
The patient should be positioned in a good light with the knee bent and apart using disposable gloves and water-soluble lubricating jelly, the labia are parted and the area are carefully examined.
2.Observations:
1. Observations at Rest:
The presence of excoriation may give an indication of the severity of incontinence. Redness and soreness extending from the perineum to the upper thighs indicates an almost continuous state of wetness.
- Examination of the introitus and distal vagina will identify the presence of vaginitis, which appears as a red, dry membrane instead of moist, pink tissue. This is more common in postmenopausal women and often mirrors the state of the urethra; urethritis may cause frequency, urgency and dysuria.
- The presence of urethrocele, cystocele, uterine prolapse and rectocele can be initially observed in this position. The presence of hemorrhoids is noted.
2.Observations During a Contraction:
A brief lesson in contracting the pelvic floor muscles should be given before muscle power is assessed. Patients are told to “squeeze and lift” the PFM as if preventing the escape of flatus and urine. During a strong contraction, the main observation is a puckering and in-drawing of the vaginal introitus, anal sphincter and perineal body; a weak contraction may only demonstrate a slight puckering, and some patients are unable to produce any movement of the perineum.
3.Observations During a Cough:
The impact of a cough on a healthy, strong pelvic floor muscles produces little or no movement, either at the vaginal introitus or the perineum as a whole. On the other hand, a patient with a very weak pelvic floor muscles may demonstrate:
- perineal descent, possibly below the level of the ischial spines.
- the vaginal introitus will bulge and gape.
- may be caudal movement of any prolapse.
- short spurt of urine may be observed.
- These observations should be relayed to the patient so that she is aware of the bulging perineum on coughing and the possible damage it may cause. In this position, the patient should be instructed to contract the pelvic floor muscles and repeat the cough, to test whether she can minimize the perineal descent.
4.Observations of Extraneous Muscle Activity:
- Isolate a pelvic floor muscles contraction is very important. however, it is common to observe a patient holding breath and contracting the abdominals, glutei and adductors in an effort to produce a maximum contraction, these extraneous muscles are generally recruited when the pelvic floor muscles are tiring.
- Observation and palpation of these auxiliary muscles will determine the extent of their involvement and the examiner should make the patient aware of these unwanted muscle contractions. This is not only to avoid undue fatigue, but contraction of the abdominal muscles produces an increase in intra-abdominal and intravesical pressure, which may produce incontinence.
3.Palpations:
Palpations can be performed per vaginum or per rectum, and this technique is used to evaluate:
- muscles bulk
- resting tone
- contractile strength
- reflex response to cough
- reduced sensation or pain should be identified
Internal Vaginal Digital Palpation:
useful tool for examination vagina, it is performed by inserting two fingers (index and middle) into the vaginal cavity.
- the therapist is looking for both a squeeze and lift when Pelvic floor muscle contraction can be felt.
PERFECT Scheme:
method of examination , developed by Laycock, involve introducing the index and middle finger into the distal 3 cm of the vagina, and assessing:
- Power: Modified Oxford Scale.
- Endurance: How long can hold a maximal voluntary contraction (up to 10sec).
- Repetitions: How many maximal voluntary contractions hold with a rest between them, up to 10 reps
(eg.: 10 repetitions of a 10-second hold).
- Fast: The number of 1 second maximal voluntary contractions can perform in a row (up to 10).
- Every Contraction
- Timed: a reminder to time every contraction.
4.Ultrasound:
used to assess pelvic floor muscles contractions and assessing movement of pelvic structures during contraction, there is two types:
- Transabdominal ultrasound: non-invasive, valid and reliable tool, the examiner can evaluate both the squeeze and lift component of the contraction by placing the ultrasound probe suprapubically.
- Real-time ultrasound: non-invasive, provides a good visual feedback tool for patients to use as a means of contracting their pelvic floor muscles correctly.
- non-invasive: can be used in patients who are not comfortable with an internal examination or where an internal examination is contra-indicated e.g., children.
5.MRI:
used to evaluate for pelvic floor muscles dysfunction as well as the ability of ittt to lift while contracting. it is very expensive and is not used widely for standard assessment.
6.Manometers and Dynamometers:
reliable tools that can measure a pelvic floor muscle contraction and may be superior to digital palpation as an objective measure of strength.
Pelvic floor muscles disorders:
Abnormal function of the pelvic floor muscles can result from excessively tight (hypertonicity) or weakened (hypotonicity) or inappropriate coordination of the pelvic floor muscles. The goal is balance, pelvic floor muscles should be strong enough to stabilize core and secure organs but flexible enough to stretch and relax.
Causes of weak pelvic floor muscles:
- injury or trauma, including childbirth and surgery.
- stressed during pregnancy or from overuse (repeated heavy lifting, chronic coughing, constipation).
- hormone changes during menopause and lose strength as a natural part of aging.
- Conditions like diabetes may also play a role in weakening pelvic floor muscles.
Weak pelvic floor muscles can lead to:
- · Urinary incontinence: involuntary leakage of urine.
- Fecal incontinence: involuntary leakage of stool (not related to sphincter disruption).
- Stress incontinence: urine or stool leakage during laugh, cough, sneeze or lift. It’s more common after childbirth, following prostate surgery or pelvis injury.
- pelvic organs prolapse:
- Uterine prolapse: herniation of the uterus via the vagina beyond the introitus.
- Vaginal prolapse: herniation of the vaginal apex beyond the introitus.
- Rectal prolapse: intussusception of the rectum beyond the anal verge (Procedentia) or proximal to the anus (Occult).
- Enterocele: bulging or herniation of the intestines into the vagina.
- Rectocele: bulging or herniation of the rectum into the vagina.
- Urethrocele (urethral prolapse): bulging of the urethra into the vagina.
- Cystocele: bulging or herniation of the bladder into the vagina (anterior).
- Perineal descent: bulging of the perineum below the boney pelvic outlet.
- Common sign and symptom of weak pelvic floor muscles is urine and fecal incontinence.
Tightness of pelvic floor muscles:
Tightness is less common; it is lead to the following condition:
- Pelvic pain: chronic pain lasting more than three to six months, unrelated to other defined conditions.
- Levator spasm: another term for chronic pelvic pain related to the levator ani musculature.
- Proctalgia fugax: fleeting spastic pain related to the levator ani musculature.
- Difficult urination: hesitancy, delay in the urinary stream.
- Dyspareunia: pain with or following sexual intercourse.
- Constipation: paradoxical contraction or inadequate relaxation during attempted defecation (dyssynergic defecation).
Causes of Tight pelvic floor muscles
- Habitually holding in urine or stool. Some people do this as children and continue the practice into adulthood. Others may do it because of their lifestyle or job.
- Injury or trauma to the pelvic muscles during surgery, pregnancy or childbirth or a traumatic accident.
- Muscular dysfunction caused by prolonged sitting, abnormal posture, irregular gait when walking or uneven pelvic bones.
- Other pain-causing conditions such as irritable bowel syndrome, endometriosis, vulvodynia, anal fissures and painful bladder syndrome.
- Sexual or physical abuse.
- Stress, depression and anxiety.
Treatments of pelvic floor muscles disorders:
1. Pelvic floor muscles exercise (PFME):
also known as pelvic floor muscle training, pelvic floor physiotherapy or pelvic floor rehabilitation, PFME is defined as exercise to improve pelvic floor muscle strength, power, endurance, relaxation, is a mainstay of behavioral treatment for urinary incontinence and overactive bladder symptoms.
first introduced by Margaret Morris in 1936 to instruct women how to exercise vaginal muscles. However, PFME was first popularized by Arnold Kegel in 1948. Over time, this exercise has evolved as a behavioral and physical therapy, into a conservative treatment for urinary incontinence.
PFME is an exercise that involves the understanding of pelvic floor muscle activation and the pursuit of a repeated PFME program over time.
effectiveness depends on regular performance of Pelvic floor muscles exercise (PFME) with proper technique. In addition to the most important factor, the patients’ adherence during the intervention and afterwards in the maintenance phase. Which lead the patients to have better outcomes.
Instructions of Pelvic floor muscles exercise:
- Contract muscles around examiner’s finger and try to pull up and in.
- Imagine trying to prevent the passing of bowel gas by tightening the ring of muscles around the anus without tensing the muscles of legs or buttocks. A closing and lifting sensation should be felt.
- Imagine moving the penis up and down without moving any other part of the body for men.
- Feel vagina and rectum pull up and in for women.
- Muscle isolation is the common problem encountered in teaching PFME. In addition, patients may substitute a straining down Valsalva maneuver, which threatens to worsen the condition of pelvic floor muscles.
2.Biofeedback therapy:
This modality involves placement of a vaginal pressure sensor within the vagina that measures pressure and provides an audible or visual feedback of strength of pelvic floor muscles contraction.
- Produces computer-generated graphs that are displayed on a monitor records pelvic floor muscle activity, the muscle contraction, relaxation, and strength.
- Helps patients find their pelvic muscles by showing changes when they squeeze or tighten the right muscle.
- Useful to reach a new level of strength in pelvic floor muscles.
- Useful in patients who are unable to properly isolate the pelvic floor muscles or use accessory muscles during pelvic floor contractions.
Biofeedback equipment with monitors for visual feedback. (A) Equipment chair. (B) Biofeedback graph showing pelvic floor muscle contraction
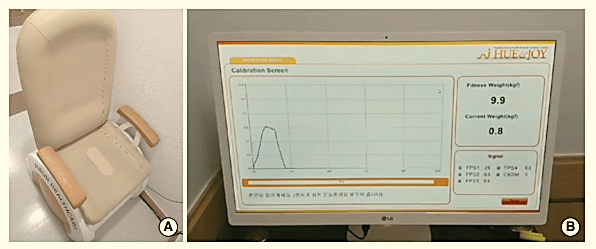
(B) Biofeedback graph showing pelvic floor muscle contraction
3.Electrical stimulation:
The device is placed in the vagina or anus and provides a small electrical current that stimulates the pelvic floor muscles to contract, aiding the patient in identification and isolation of the proper muscles
- Long-term or chronic electrical stimulation delivered below the sensory threshold aiming at detrusor inhibition by afferent pudendal nerve stimulation.
- maximal electrical stimulation, using a high-intensity stimulus (just below the pain threshold), aims to improve urethral closure by direct and reflexogenic contraction of striated peri-urethral musculature.
4.vaginal weighted cone:
Method helps patients identify and control their pelvic floor muscles.
- inserts the cone in vagina and uses pelvic muscle contractions to hold it in place during activity.
- When a weighted cone is placed in the vagina while standing, the sensation of “losing the cone” provides strong sensory feedback that prompts the pelvic floor muscle to contract to prevent it from slipping out.
5.Breathing and relaxation exercises
6.Postural correction exercises and re-education.
7.Treatment with acupuncture.
8.Medications for anxiety, pain, constipation or frequent urination.
9.Treatment another causes of back pain
NOTE:
- Hypertonicity (unable to relax) of pelvic floor muscles treated at first and then the hypotonicity, strengthening exercises may exacerbate the symptoms. It is difficult to initiate or activate hypertonic pelvic floor muscles if they are not able to relax towards the basic resting tone.
Prevention:
Understanding the contraction and relaxation of pelvic floor muscles can reduce risk of disfunction. in addition to:
- mindfulness and relaxation techniques.
- Practice pelvic floor exercises during and after pregnancy.
- Avoid constipation and straining.
- Seek medical care when having pelvic or anal pain.
- Avoid prolonged periods of holding poop and pee.
Reference:
- Petty, N. J., & Ryder, D. (2018). Musculoskeletal examination and assessment: A handbook for therapists. Elsevier.
- Singh, V. (2014). Textbook of Anatomy: Abdomen and Lower Limb, Volume Ii, 2e . Elsevier.
- Schüssler Bernard, Laycock, J., Norton, P. A., & Stanton, S. L. (1994). Pelvic floor re-education: Principles and practice. Springer London.
- Cleveland Clinic. (n.d.). Pelvic floor muscles: Anatomy, function & conditions. Cleveland Clinic. Retrieved October 20, 2022, from https://my.clevelandclinic.org/health/body/22729-pelvic-floor-muscles
- Kearney, R., Sawhney, R., & DeLancey, O. L. (2004). Levator Ani Muscle Anatomy Evaluated by Origin-Insertion Pairs. Obstetrics and gynecology, 104(1), 168.(https://doi.org/10.1097/01.AOG.0000128906.61529.6b)
- Pelvic Floor Muscle Function and Strength. (2019, August 25). Physiopedia, . Retrieved 12:30, October 22, 2022 from https://www.physio-pedia.com/index.php?title=Pelvic_Floor_Muscle_Function_and_Strength&oldid=220450.
- Grimes, W. R., & Stratton, M. (2022). Pelvic Floor Dysfunction. In StatPearls. StatPearls Publishing. ( https://pubmed.ncbi.nlm.nih.gov/32644672/ )
- Shannon L. Wallacea , Lucia D. Millerb , & Kavita Mishraa.( 2019). Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Wolters Kluwer Health, Inc. Volume 31.